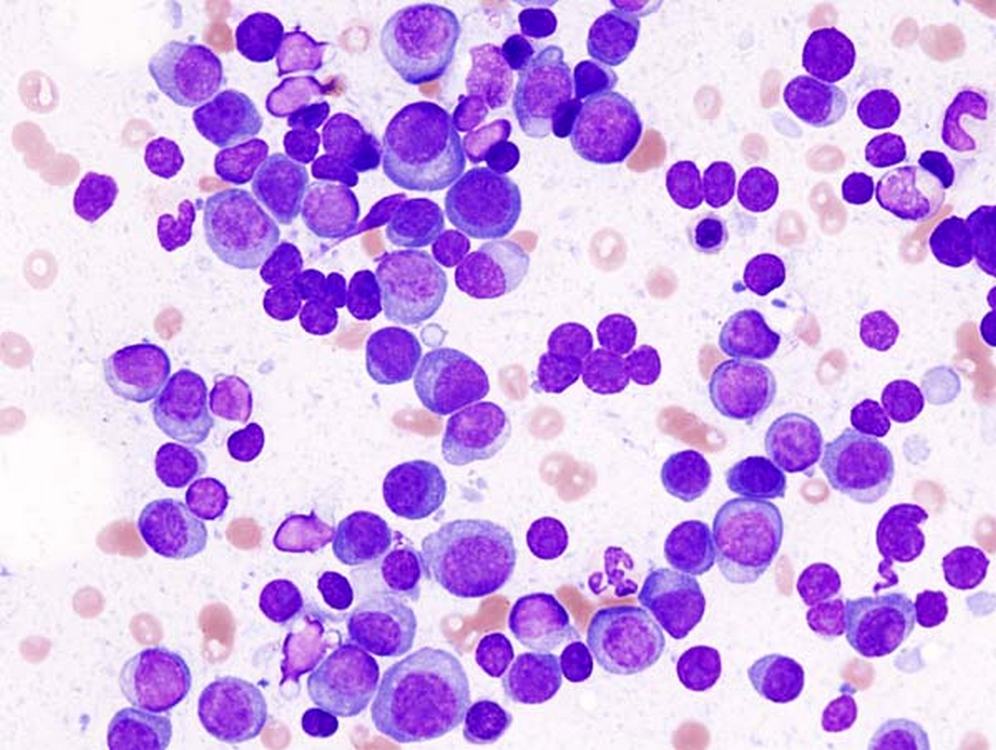
In a pair of groundbreaking studies, scientists replicated a time-consuming, laboratory-based, cancer therapy within myeloma patients’ own bodies.
If standardized, such an advancement would allow for one of the most successful non-chemo cancer treatments to be done both faster and cheaper.
CAR T-cell therapy involves retrieving a patient’s immune system component called a T-cell and using a virus to genetically add the CAR, or chimeric antigen receptor, to it. This process is done in a lab—typically outside the hospital where the patient is being treated—before the cells are shipped back for transplant.
The alteration allows T-cells to home in on cancer cells directly by penetrating the biological stealth capabilities tumors have, but is also expensive and laborious. If, scientists have considered in the last decade, the process could be done inside the body, it would save lives that are sometimes lost waiting out the month-or-so-long process it takes to alter the T-cells in the lab.
That’s exactly what’s been established in a pair of recent trials, the results of which were just presented at the American Society of Hematology’s (ASH) annual meeting.
In the team’s first trial in July, 4 patients with multiple myeloma, a kind of blood cancer, had their T-cells engineered in vivo with the CAR gene. They produced the altered cells, which successfully attacked the tumors in their bone marrow.
2 of the patients seemed to be cured, with the cancer cells no longer detectable in their bone marrow, and a tell-tale circulating blood protein also absent from their bodies. 2 others didn’t benefit to that extent, but appeared to be in remission after 5 months.
“The question is no longer can you really do this,” Yvonne Chen, a cancer immunotherapy researcher at UCLA, told Science News. “The question now is can you reach the level of efficacy that’s expected and will the safety profile meet the target.”
On the question of safety, the patients suffered from significant side effects, likely due to the effects of the deactivated virus used to reprogram their T-cells, which has been known to trigger flu-like symptoms that have even been fatal on occasion with the lab-based CAR T-cell method.
Interestingly, the flu-like inflammation was very mild in all 4 patients, who instead suffered from drops in blood pressure, lack of oxygen, and mental confusion. All recovered following the treatment process.
CAR T-CELL THERAPY AT WORK: Christmas ‘Miracle’ for 6-Year-Old with Leukemia Who’s Now Thriving After T-cell Therapy Instead of Chemo
In the second trial, another 4 patients with previously untreatable multiple myeloma had no detectable cancer cells in their bone marrow 1 month after treatment, a status maintained in one patient 5-months post-treatment. The side effects were less substantive for unknown reasons.
“I think it gives us a glimpse into the future,” said hematologist Joy Ho of the Royal Prince Alfred Hospital. “In vivo CAR-T for multiple myeloma is here and hopefully it will stay.”
CANCER IMPROVEMENTS: Oncologists Treat Patient’s Rare Cancer with Isolated Chemotherapy Delivery, Preventing Side-Effects
CAR T-cell therapy is also being looked at as a treatment for non-cancer diseases like autoimmune disorders. The lab-based process not only takes a month, but costs hundreds of thousands of dollars, and requires a particularly aggressive chemotherapy session to wipe out the existing T-cells before receiving the new, altered ones.
If the in vivo process can be rendered safer, it would allow hundreds more patients to access it, and save hundreds of lives.
Cancer Research Gets Better And Better: LET YOUR FRIENDS KNOW…