A new study proposes a strategy for reversing the memory problems that accompany Alzheimer’s disease and related dementias, exploring an alternative to the laser-focused approach of big pharma to target toxic tau proteins known to go hand in glove with these diseases.
Rather than remove the damaging compound, scientists at the Buck Institute for Research on Aging aimed to reverse the damage the compound caused using an innate protein found in the kidneys and the brain.
“While newly approved drugs for Alzheimer’s show some promise for slowing the memory-robbing disease, the current treatments fall far short of being effective at regaining memory. What is needed are more treatment options targeted to restore memory,” said Buck Assistant Professor Tara Tracy, PhD, the senior author of the study.
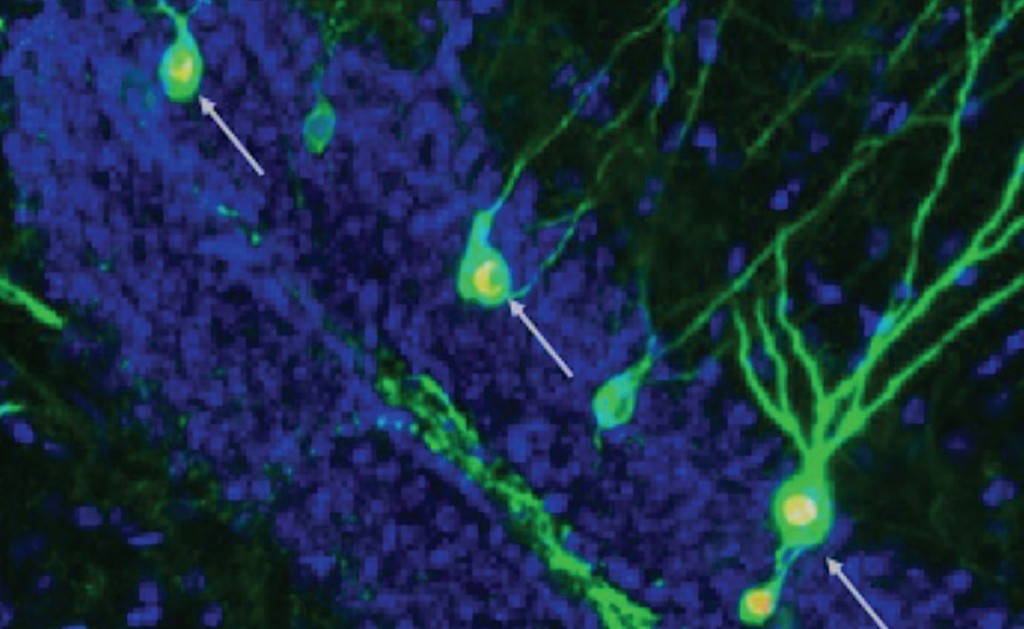
The protein in question is called KIBRA, named because it is found in the kidney and the brain. Along with being produced in the kidney, Tracy and her team identified its presence throughout brain synapses, which are the connections between neurons that allow memories to be formed and recalled.
They also found that KIBRA is deficient in the brains of people with Alzheimer’s and dementia.
“We wondered how the lower levels of KIBRA affected signaling at the synapse, and whether understanding that mechanism better could yield some insight into how to repair the synapses damaged during the course of Alzheimer’s disease,” said Buck Staff Scientist Grant Kauwe, Ph.D., co-first author of the study.
“What we identified is a mechanism that could be targeted to repair synaptic function, and we are now trying to develop a therapy based on this work.”
To figure out how KIBRA affects synapses, the team created a shortened functional version of the KIBRA protein. In laboratory mice that have a condition mimicking human Alzheimer’s disease, they found that this protein can reverse the memory impairment associated with this type of dementia. They found that KIBRA rescues mechanisms that promote the resilience of synapses.
MORE DEMENTIA STORIES OF HOPE: New Alzheimer’s Drug Slows Mental Decline By 27% in Trial Hailed as ‘Most Encouraging to Date’
The team next wanted to measure the levels of KIBRA in the cerebrospinal fluid of humans to understand how it changed along with other key markers in Alzheimer’s, such as toxic tau protein or beta-amyloid. They found that higher levels of KIBRA in the cerebrospinal fluid, but lower levels in the brain, corresponded to the severity of dementia.
“We also found this amazing correlation between increased tau levels and increased KIBRA levels in the cerebrospinal fluid,” said Tracy. “It was very surprising how strong the relationship was, which really points to the role of KIBRA being affected by tau in the brain.”
The team is exploring this phenomenon further, in hopes that KIBRA could be used as a biomarker of synaptic dysfunction and cognitive decline that could be useful for diagnosis, treatment planning, and tracking disease progression and response to therapy.
RELATED: Electrical Brain Stimulation Improves Mental Processes in Alzheimer’s Patients
“Interestingly, KIBRA restored synaptic function and memory in mice, despite not fixing the problem of toxic tau protein accumulation,” said Kristeen Pareja-Navarro, co-first author of the study. “Our work supports the possibility that KIBRA could be used as a therapy to improve memory after the onset of memory loss, even though the toxic protein that caused the damage remains.”
While addressing the root cause of a disease, in this case the tau protein, would in theory be the more desirable treatment method, almost all pharmacological options for doing so have failed to demonstrate robust success in diminishing the symptoms of Alzheimer’s.
These repeat failures give the impetus for seeking another approach.
SHARE This Important Development With Your Friends On Social Media…




















