A team of scientists at the Salk Institute have found that a particular kind of immunotherapy was able to train the brain’s ‘invisible scalpel’ on an incurable form of brain cancer in mice.
Glioblastoma is the most common form of brain tumor, and while it’s also the most deadly, our brains come equipped with the immune cells needed to destroy them.
The problem is, cancer tumors have mechanisms that allow them to evade the detection of the immune system. That’s where immunotherapy comes in. While not universally effective, many tumors can be treated or even cured by immunotherapy, which helps the immune system see through these evasive mechanisms and destroy the cancer.
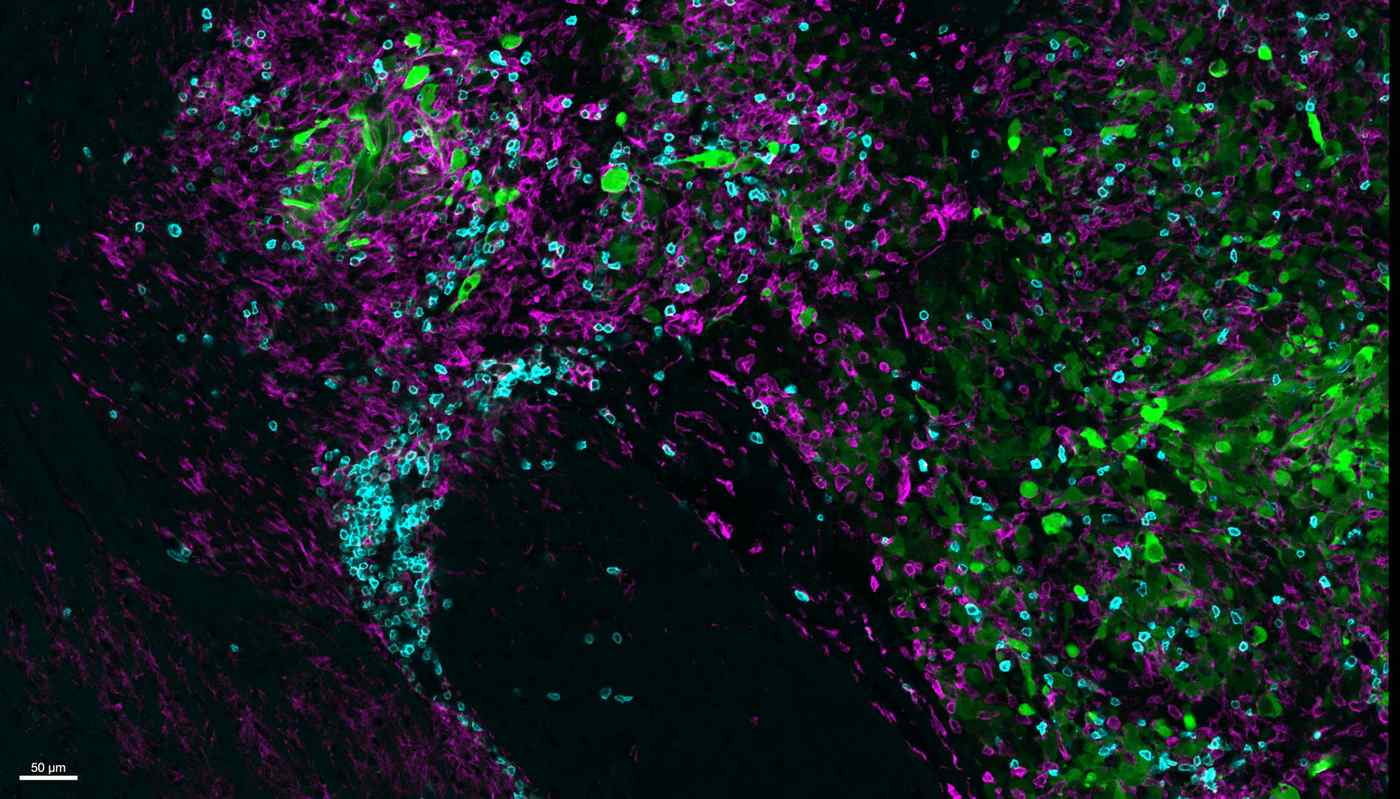
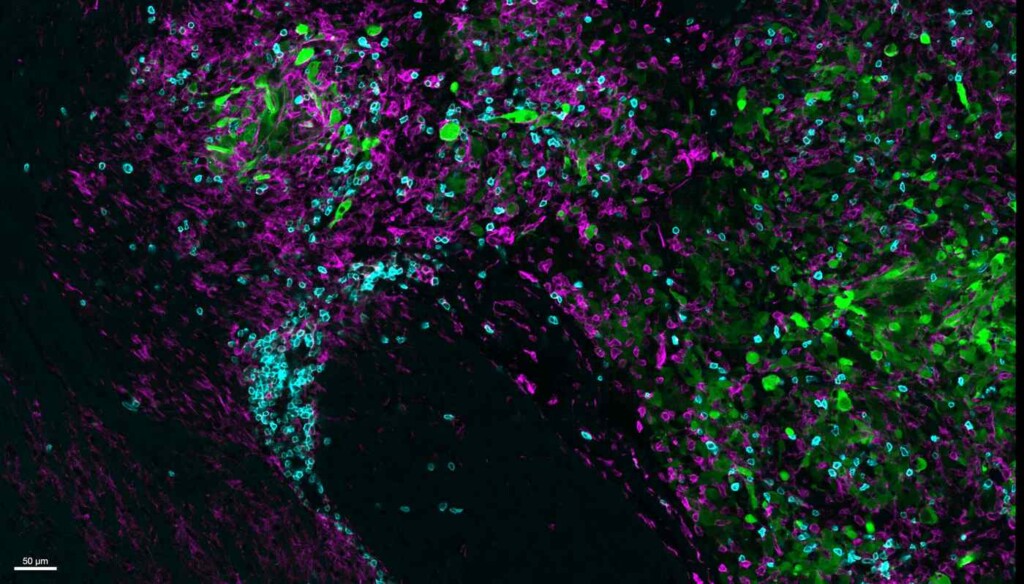
Professor Susan Kaech, director of the NOMIS Center for Immunobiology and Microbial Pathogenesis, led a team to investigate whether immunotherapy could be used on glioblastomas by experimenting with an immunotherapy drug called anti-CTLA-4 and two specialized immune cells called CD4+ T cells and microglia respectively.
“There are currently no effective treatments for glioblastoma—a diagnosis today is basically a death sentence,” says Professor Susan Kaech, senior author of the paper published in the journal Immunity.
“We’re extremely excited to find an immunotherapy regimen that uses the mouse’s own immune cells to fight the brain cancer and leads to considerable shrinkage, and in some cases elimination, of the tumor.”
Both anti-CTLA-4 and CD4+ T cells have been overlooked or unfavored in clinical research on account of there being more effective alternatives identified in the early years of immunotherapy research.
MORE FROM SALK: Resetting Clock on Aging Cells Safely Reversed Signs of Decline in Mice
Regarding anti-CTLA-4, the more-effective alternative, PD-1, never worked in glioblastoma models. Anti-CTLA-4, however, does—by blocking cells from making the CTLA-4 protein, which, if not blocked, inhibits CD4+ T cell activity.
The researchers found that by allowing T cell activity to take place, CD4+ T cells secreted a protein called interferon-gamma that caused the tumor to throw up “stress flags” while simultaneously alerting microglia. A specially adapted immune cell for the brain environment, they started eating up these stressed tumor cells.
Each stressed-out cell the microglia ate led the tumor to create more interferon-gamma, leading to more consumption until the whole tumor was devoured.
MORE CANCER TREATMENTS: Immunotherapy Drugs So Effective that Tumors Disappear in Weeks for Head and Neck Cancer Patients in Landmark Trial
“We were stunned by this novel codependency between microglia and CD4+ T cells,” says co-first author Siva Karthik Varanasi, a postdoctoral researcher in Kaech’s lab. “We are already excited about so many new biological questions and therapeutic solutions that could radically change treatment for deadly cancers like glioblastoma.”
Next, the researchers will examine whether this cancer-killing cell cycle is present in human glioblastoma cases. Additionally, they aim to look at other animal models with differing glioblastoma subtypes, expanding their understanding of the disease and optimal treatments.
SHARE This Big Brain Cancer Breakthrough On Social Media…