While the original CRISPR gene editing technology could only target 12.5% of the human genome, a new method developed by engineers at Duke University expands access to nearly every gene to potentially target and treat a broader range of diseases.
The study published in the journal Nature Communications, involved collaborators at Harvard University, Massachusetts Institute of Technology, University of Massachusetts Medical School, University of Zurich, and McMaster University.
“With this new tool, we can target nearly 100% of the genome with far more precision,” said Pranam Chatterjee, Assistant Professor of Biomedical Engineering at Duke.
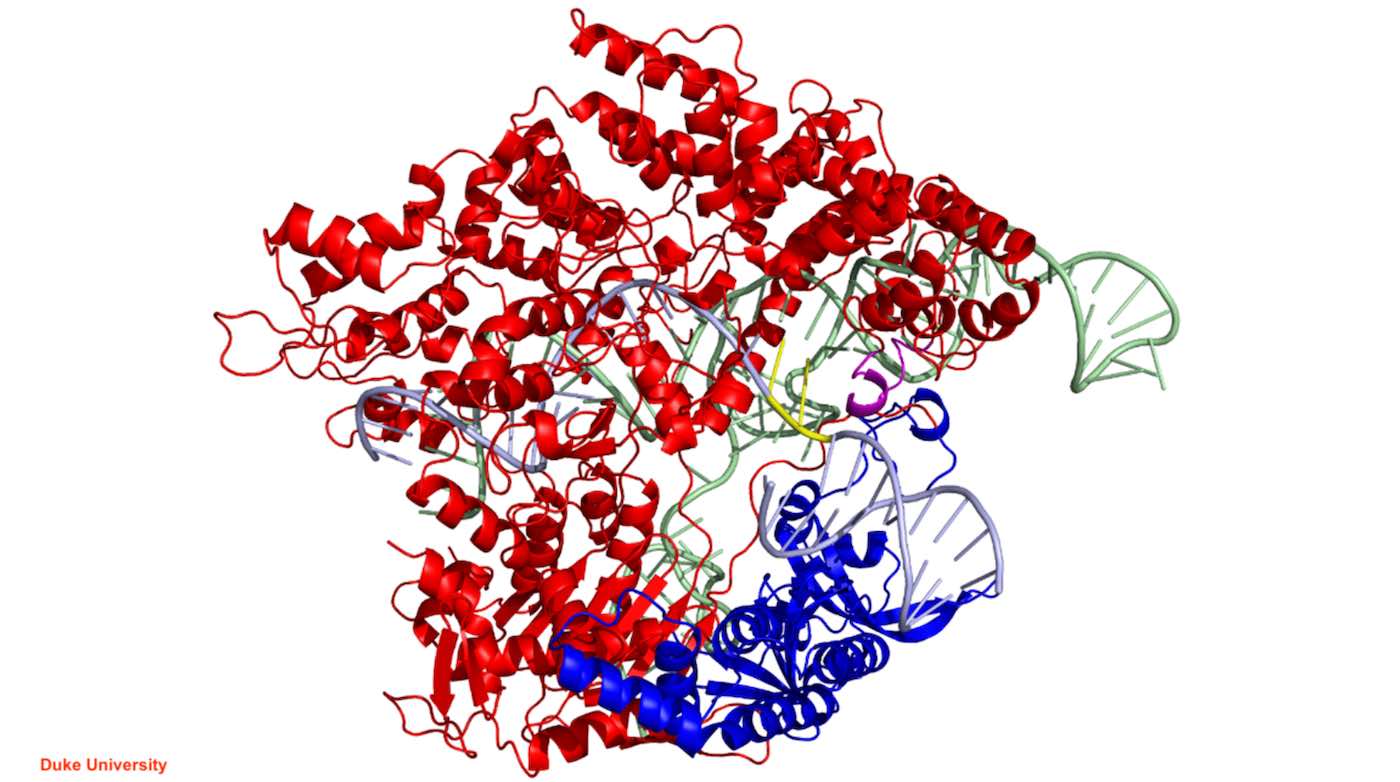
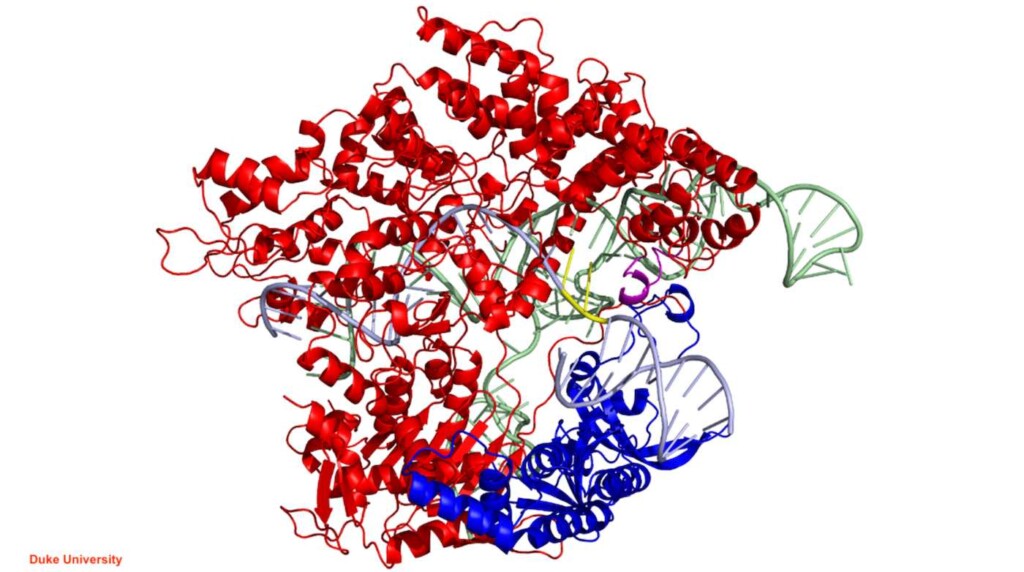
CRISPR-Cas is a bacterial immune system that allows bacteria to use RNA molecules and CRISPR-associated (Cas) proteins to target and destroy the DNA of invading viruses. Since its discovery, researchers have raced to develop an arsenal of new CRISPR systems for applications in gene therapy and genome engineering.
The team investigated the new tool’s potential therapeutic uses for genetic diseases that were untreatable with the standard CRISPR system. Their first test was Rett syndrome, a progressive neurological disorder that predominantly affects young females and is caused by one of eight mutations to a specific gene.
The second was Huntington’s disease, a rare, inherited neurological disorder that causes the degeneration of neurons in the brain. Using the new technology, the team was able to alter previously inaccessible mutations, providing potential therapeutic opportunities for both diseases.
SUCCESS SO FAR: FDA Approves Cure for Sickle Cell Disease, the First Treatment to Use Gene-Editing Tool CRISPR
How Does it Work?
To make edits to the genome, Cas proteins utilize both an RNA molecule, which guides the enzyme to a targeted stretch of DNA, and a protospacer adjacent motif, or PAM, which is a short DNA sequence that immediately follows the targeted DNA sequence and is required for the Cas protein to bind.
Once a guide RNA finds its complementary DNA sequence and the Cas enzyme binds the adjacent PAM, the enzyme acts like scissors to make a cut in the DNA, triggering the desired changes to the genome. The most common CRISPR-Cas system is the Cas9 from Streptococcus pyogenes bacteria (SpCas9), which requires a PAM sequence of two guanine bases (GG) in a row.
In previous work, Chatterjee and his team used bioinformatics tools to discover and engineer new Cas9 proteins, including Sc++, which only requires a single guanine base PAM to make a cut. This change made it possible for researchers to edit nearly 50% of all DNA sequences.
WHAT ELSE CAN IT DO? CRISPR Gene Editing Reverses ‘Permanent’ Vision Loss in Mice
At the same time, Chatterjee’s collaborators at Harvard, led by Benjamin Kleinstiver, an assistant professor at Harvard Medical School, engineered a separate variant called SpRY. While SpRY could bind to any one of the four DNA bases that could form the PAM, it had a much stronger affinity for adenine and guanine.
Because both systems had drawbacks, the group decided to put the best of both together into a new variant called SpRyc.
While SpRYc was slower than its counterparts at cutting target DNA sequences, it was more effective than both the traditional enzymes at editing specific sections of DNA. Despite SpRYc’s broadness, it was also more accurate than SpRY.
INCREDIBLE NEWS: Aggressive Leukemia Disappears in 13-Year-old Who was First to Receive New CRISPR Treatment
“There is a lot of potential with SpRYc, whether it’s exploring how to translate it into the clinic or finding ways to make it even more efficient,” said Chatterjee. “We look forward to exploring the full capabilities of our tool.”
(Source: Duke University)
EXCITING STUFF to Share For the New Year on Social Media…