Mosquitoes are one of the deadliest animals on the planet because they spread yellow fever, dengue, encephalitis, and malaria, which killed 400,000 people in 2019.
Now, clinical trials of the promising R21 vaccine in Burkina Faso may be an effective tool against the disease, as it triggers the body’s immune system to attack the parasite—and has been 77% effective in phase 2 trials.
Ravaging and replicating through the body in seven different stages, malaria comes from the parasite Plasmodium falciparum, which isn’t a particularly good candidate for vaccination (mosquito nets are still the most effective measure), due to constant evolution throughout its life cycle. For perspective, it’s made from 5,000 genes, while the coronavirus that’s impacted all our lives contains just 16.
In the ’80s, the pharmaceutical company GlaxoSmithKline attempted to use vaccination to tackle the malaria epidemic by targeting the initial stage of the Plasmodium life cycle, called a sporozoite. In 1983, according to National Geographic, researchers discovered that sporozoites are covered in proteins that provoke a strong immune system response, but the evolution to their next life cycle occurs too fast for natural immunity to recognize and terminate the sporozoites.
The idea was to make a carrier that would present a kind of sporozoite protein-punching bag, so that when the real thing arrived the immune system would react fast enough to eradicate it before it spread to the liver.
Marketed commercially as Mosquirix, it’s the single-most tested vaccine candidate for malaria, but after twelve months, its effectiveness falls to less than sleeping under mosquito nets.
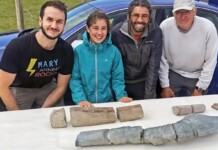
Halidou Tinto, an epidemiologist and expert in Malaria, works near the Burkina Faso capital of Ouagadougou and helped to organize a trial of 450 children between 5-17 years of age for the new R21 vaccine, that uses the same method as Mosquirix, but simply manufactured better—where before only one in five proteins were coated in the sporozoite protein, R21 made that five in five.
At its best, R21 reduced clinical malaria incidence by 77%, 2% more than the 75% target set out by the WHO in 2013 as part of an international attempt to push the global malaria problem more into mainstream pharmacology. There was no difference in malaria incidence at a 6 or a 12-month follow-up; a significant improvement over the old GSK vaccine.
The authors of this paper noted that the vaccine doses were administered in the lead up to the annual rainy season, when malaria cases spike, but that it would be worth comparing results from trials carried out at different times of the year.
RELATED: U.S. Department of Defense Funds New Lyme Disease Vaccine Development
“We are enthusiastic, but we still need phase three trials to confirm the efficacy and the safety of the vaccine before we move on,” Tinto tells National Geographic.
SHARE the Hope—Send This Story to Friends…